Background
Today I Get God Article about low grade Astrocytoma from this web http://emedicine.medscape.com/article/1156429-overview.Low-grade astrocytomas are a heterogeneous group of intrinsic central nervous system (CNS) neoplasms that share certain similarities in their clinical presentation, radiologic appearance, prognosis, and treatment. The most common intrinsic brain tumor, glioblastoma multiforme, is high grade and malignant. This contrasts with low-grade astrocytomas, which are less common and therefore less familiar to practitioners. The strategies for diagnosis and treatment are also more controversial.
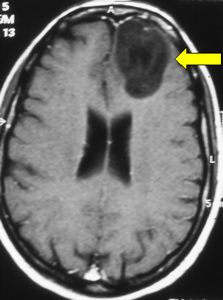
Improvements in neuroimaging permit the diagnosis of many low-grade astrocytomas that would not have been recognized previously. Low-grade astrocytomas are, by definition, slow growing, and patients survive much longer than those with high-grade gliomas. Proper management involves recognition, treatment of symptoms (eg, seizures), and surgery, with or without adjunctive therapy. Low-grade astrocytomas are found in both the brain and the spinal cord.
Pathophysiology
Low-grade astrocytomas are primary tumors (rather than extraaxial or metastatic tumors) of the brain. Astrocytomas are one type of glioma, a tumor that forms from neoplastic transformation of the so-called supporting cells of the brain, the glia or neuroglia. Gliomas arise from the glial cell lineage from which astrocytes, oligodendrocytes, and ependymal cells originate. The corresponding tumors are astrocytomas, oligodendrogliomas, and ependymomas. Grading of a glioma is based on the histopathologic evaluation of surgical specimens. Several classification schemes have been proposed.The World Health Organization (WHO) scheme is based on the appearance of certain characteristics: atypia, mitoses, endothelial proliferation, and necrosis. These features reflect the malignant potential of the tumor in terms of invasion and growth rate. Tumors without any of these features are grade I, and those with one of these features (usually atypia) are grade II. Tumors with 2 criteria and tumors with 3 or 4 criteria are WHO grades III and IV, respectively. Thus, the low-grade group of astrocytomas are grades I and II.
A subset of astrocytomas, because of their distinctive pathology, preclude the use of the usual 4-featured grading system. These tumors may have endothelial proliferation and marked atypia; nevertheless, they are slow growing and well circumscribed. This subset comprises juvenile pilocytic astrocytoma (JPA) and its variant a juvenile pilomyxoid astrocytoma, pleomorphic xanthoastrocytoma (PXA), and subependymal giant-cell astrocytoma (SGCA). Low-grade astrocytomas generally cause symptoms by perturbing cerebral function (eg, seizures), elevating intracranial pressure (ICP) by either mass effect or obstructing cerebrospinal fluid (CSF) pathways (ie, hydrocephalus), or causing neurologic (and sometimes endocrine) abnormalities (eg, paralysis, sensory deficits, aberrant behavior, headaches).
Infiltrating low-grade astrocytomas tend to occur in the lobes of the cerebral hemispheres, especially in the frontal lobe. Pilocytic astrocytomas may occur in the frontal, temporal, and parietal lobes and cerebellum, but they are also common in locations closer to the midline, such as the hypothalamus, thalamus, optic chiasm, and brain stem. In children, pilocytic astrocytomas have a predilection for the mesial structures of the cerebellum. Pleomorphic xanthoastrocytomas also are found most commonly in the hemispheres, particularly the temporal lobes. Subependymal giant-cell astrocytomas are found most commonly in the lateral wall of the third ventricle and almost exclusively in patients with tuberous sclerosis.
Frequency
United States
The yearly incidence of gliomas in adults in the United States is approximately 5.4 cases per 100,000 population. Low-grade tumors make up approximately 10-20% of these tumors in adults and 25% in children. Thus, the incidence in adults of low-grade gliomas is about 0.8 case per 100,000 population. The incidence of gliomas in children is approximately 2.4 cases per 100,000 population, making the incidence of low-grade gliomas 0.6 case per 100,000 population.Gliomas are associated with certain phakomatoses, especially neurofibromatosis type 1 (NF-1). Low-grade astrocytomas occur more commonly in these patients, particularly in the optic nerve and chiasm. Patients with tuberous sclerosis have a host of cerebral anomalies, accounting for the high incidence of mental retardation. Subependymal giant-cell astrocytomas are found almost exclusively in patients with tuberous sclerosis.
International
The incidence of low-grade astrocytoma has not been shown to vary significantly with nationality. However, studies examining the incidence of malignant CNS tumors have shown some variation with national origin. Since some of these high-grade lesions arise from low-grade tumors, these trends are worth mentioning. Specifically, the incidence of CNS tumors in the United States, Israel, and the Nordic countries is relatively high, while Japan and Asian countries have a lower incidence. These differences probably reflect some biological differences as well as differences in pathologic diagnosis and reporting.Mortality/Morbidity
Differences in patient populations, diagnostic methods, and reporting make defining the exact median survival duration for all patients with low-grade astrocytomas difficult. This is complicated by the fact that low-grade astrocytomas, as discussed already, are a heterogeneous group of tumors. However, the median survival duration of patients with low-grade astrocytomas is approximately 7.5 years.- In a recent series, taking all patients, the 5-year survival rate ranged from 65-80%, while the 10-year survival rate varied from 20-45%. Several factors influence survival. For example, the histopathology of the tumor has a clear influence on prognosis. Patients with grade I lesions have better survival rates than those with grade II lesions. Younger age and better performance status at the time of diagnosis also have a positive influence on long-term survival.
- The type of therapy received also influences outcome. Total resection has been shown in numerous studies to be associated with better survival rates than other therapeutic modalities. This is partially due to the fact that complete resection is more easily accomplished in well-circumscribed, slower-growing tumors. However, sound oncologic principles also suggest that cytoreduction offers benefit. Radiation probably prolongs survival in patients whose tumors are resected incompletely. However, the survival advantage conferred by chemotherapy remains to be demonstrated clearly.
- Over periods of many years, these tumors frequently undergo dedifferentiation into higher-grade lesions. Such lesions then grow more rapidly and eventually become fatal. Progressive neurologic deficit is the norm as the tumor increases in size. Even lesions that do not dedifferentiate but continue to grow can cause death ultimately, primarily as a result of mass effect that may result in cerebral herniation and brainstem dysfunction.
Race
No clear evidence has been published in the literature that low-grade astrocytomas are more common in any racial or ethnic group. In the United States, malignant CNS tumors are slightly more common in whites than in blacks. Whether this applies to low-grade tumors as well remains to be shown.Sex
In most series, a slight male predominance (55%-65%) has been noted, and this difference generally applies to gliomas of all types and grades.Age
The median age of patients diagnosed with a low-grade astrocytoma, approximately 35 years, is younger than that of patients with more malignant gliomas. Juvenile pilocytic astrocytomas have a median age at diagnosis about a decade younger than other low-grade astrocytomas. This may account for the positive influence on survival duration in some series in which the pilocytic phenotype is associated with an improved outcome. The incidence of primary brain tumors, malignant astrocytomas in particular, is increasing in elderly patients.1Clinical
History
No historical factors are pathognomonic for low-grade glioma. The history, however, should alert the clinician to the presence of a neurologic disorder and the need for an imaging study. Putting together the information from the history, the physical examination, and the imaging data will lead to a tentative diagnosis of low-grade glioma. The histories of patients with low-grade glioma are strangely similar. With low-grade astrocytomas, the most common complaints in the history are seizure and headache. Infiltrating low-grade astrocytomas can cause focal neurologic deficits (ie, weakness or numbness). Generally, these symptoms have a gradual onset.- Pilocytic astrocytomas tend to be midline and may cause symptoms related to this location. A large cerebellar tumor can cause obstructive hydrocephalus, and the patient may present with headache and lethargy. These patients may also have a history of imbalance, falling, or incoordination. Pilocytic tumors in the brain stem cause neurologic deficits secondary to the involvement of brainstem nuclei, while hypothalamic tumors cause a variety of endocrine problems (eg, hypernatremia). Brainstem symptoms may include double vision or facial weakness. Persons with optic nerve tumors may present with visual deficits.
- Subependymal giant-cell astrocytomas frequently cause obstructive hydrocephalus in patients with tuberous sclerosis. Headache is then secondary to hydrocephalus and elevated intracranial pressure.
- Patients with pleomorphic xanthoastrocytoma frequently have long-standing histories of seizures in addition to the more general complaints already noted.
- A small percentage of low-grade astrocytomas present in the spinal cord of both children and adults. The history is characterized by a slow onset of back pain and neurologic deficits. The pain usually is localized over the region of the tumor, which is most common in the cervicothoracic area. Neurologic symptoms include paresthesias in the arms or legs. Weakness, objective numbness, and bowel or bladder symptoms also may be present.
Physical
A thorough neurologic examination is mandatory. Level of consciousness should be noted first. Lethargy is an important sign of elevated intracranial pressure. Examination of the cranial nerves may indicate involvement of the brain stem. Nystagmus is an important sign. Papilledema can be seen if intracranial pressure is elevated. The motor and sensory examination may show weakness or impairment of sensory discrimination if the motor or sensory pathways are involved with tumor, edema, or mass effect. Hemiparesis may be accompanied by increased deep tendon reflexes or an extensor plantar response (Babinski sign). Examining for cerebellar signs (eg, ataxia) is important if a tumor in that location is suspected.- Since low-grade astrocytomas are associated with some genetic disorders, examining patients for these diseases is important. Patients with tuberous sclerosis have decreased intelligence and a characteristic skin lesion on the face (around the nose) called adenoma sebaceum, which is actually angiofibroma. Other cutaneous manifestations also may be present (eg, ash-leaf spots). Patients with NF-1 may have obvious cutaneous neurofibromas and/or café-au-lait spots.
- Low-grade astrocytomas that affect the spinal cord may result in various degrees of weakness and/or sensory change in the arms, legs, or sacral area. Myelopathy with increased deep tendon reflexes and/or positive Babinski sign may be present.
Causes
The etiology of low-grade gliomas is poorly understood. High-grade gliomas, which are much more common, have been studied in greater detail regarding possible environmental factors. Environmental factors that are linked with a higher incidence of high-grade gliomas include exposure to radiation or N- nitroso compounds. These factors have been verified in experimental models; however, the degree to which these factors play a role in the incidence of human tumors is unclear.Neoplastic transformation is thought to be a genetic process, and deletions and mutations in certain genes are thought to play a role in the change of normal glial precursor cells to gliomas. For example, p53 mutations have been found in some, but not all, low-grade gliomas. Chromosomal analysis also has shown gain or loss of genetic material in certain low-grade gliomas, although as yet no consistent pattern has been appreciated. Patients with NF-1 are known to have an abnormality on chromosome 17, while the exact genetic defect in tuberous sclerosis still is being investigated.
In summary, the environmental or genetic factors that are involved in the generation of low-grade gliomas are unknown. As mentioned already, however, patients with NF-1 or tuberous sclerosis are at much higher risk of developing these tumors and should undergo surveillance imaging by MRI.
More on Low-Grade Astrocytoma |
 Overview: Low-Grade Astrocytoma Overview: Low-Grade Astrocytoma |
| Differential Diagnoses & Workup: Low-Grade Astrocytoma |
| Treatment & Medication: Low-Grade Astrocytoma |
| Follow-up: Low-Grade Astrocytoma |
| Multimedia: Low-Grade Astrocytoma |

Tidak ada komentar:
Posting Komentar